
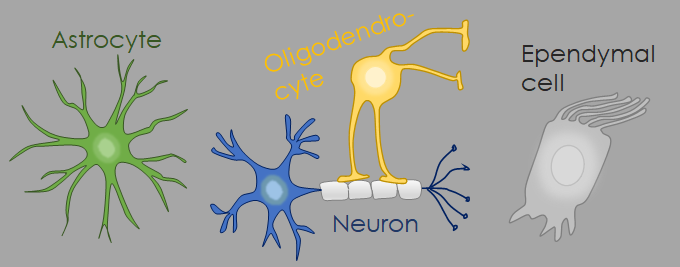
In radiological reports the term” glioma” gets thrown around a lot, but what is a glioma? A glioma isn’t just one tumor. The gliomas are a large and heterogeneous group of tumors. What these tumors have in common as that they all seem to derive from glial cells, the helper cells of the brain, such as astrocytes, oligodendrocytes or ependymal cells. Gliomas can occur at all ages, and depending on the type they can be benign (WHO 1) or highly malignant (WHO 4). In the most recent WHO-classification, tumors containing neoplastic neuronal cells were also added to the group of gliomas. The gliomas and (glio)neuronal tumors are divided into several groups: diffuse gliomas, circumscribed gliomas, (glio)neural tumors and ependymal tumors.
Diffuse gliomas are tumors that have no sharp borders and diffusely infiltrate the brain parenchyma. These tumors may look sharply demarcated on MR-images, but pathologically they aren’t. As a consequence, these tumors have a tendency to recur, even if the surgery looks complete. These tumors also have a tendency to undergo malignant transformation, even when they are low grade (WHO II), so they are never innocent. Different types of diffuse gliomas are seen in children and adults, and the diffuse gliomas are divided into “adult type diffuse gliomas”, which includes glioblastoma, astrocytoma, and oligodendroglioma (see figure below); and “pediatric diffuse gliomas”, which includes a lot of tumors with difficult names of which the most important one is probably the so-called “H3K27M-mutant midline glioma”. A H3K27M-mutant midline glioma is a highly malignant tumor, mainly seen in the brainstem of pediatric patients.

Circumscribed gliomas (or circumscribed astrocytic tumors, because the members of this group are all astrocytic tumors) are characterized by well-delineated margins on pathology and lack infiltration of the neighbouring brain parenchyma. As a consequence surgery is often curative. Circumscribed gliomas are mainly (but not exclusively) found in children.
Pilocytic astrocytoma is the most common tumor belong to this group, and is also the most frequent cerebellar tumor in children. The textbook presentation of a pilocytic astrocytoma is of a cyst containing an enhancing mural nodule (see figure below for an example of a textbook pilocytic astrocytoma).
Other circumscribed astroctyomas are the subependymal giant cell astrocytoma (SEGA), an intraventricular tumor occuring near the Monro foramen in children with tuberous sclerosis, and the pleomorphic xanthoastrocytoma, a cortical tumor that is mostly found in temporal lobe of children and young adults and often associated with chronic refractory epilepsy.

(Glio)neuronal tumors are tumors containing neoplastic neurons (neuronal tumors) or a combination of neoplastic neurons and neoplastic glial cells (glioneuronal tumors). (Glio)neuronal tumors are not very frequent and a lot of the tumors beloning to this group are rare The best known members of this group are probably gangliogliomas and dysembryoplastic neuroepithelial tumors (DNETs).
Gangliogliomas and DNETs are benign (WHO 1) tumors that can (theoretically) arise anywhere in the CNS, but are mostly found in the cortex of the temporal lobe and are typically associated with refractory temporal lobe epilepsy. Think of DNET or ganglioglioma when you’re dealing with a cortical temporal lobe tumor in a child or young adult with refractory epilepsy. The textbook appearance of a gangliogloma is of a cystic tumor with an enhancing nodule.
On the T2-weighted images below we see a typical DNET in the uncus of the left temporal lobe of a young adult with refractory epilepsy. DNETs are typically located in the cortex and often have a multicystic appearance, sometimes referred to as a “bubbly soap” appearance.

Ependymal tumors are tumors that are derived from ependymal cells. The “ependymal tumor” group consists of: fossa posterior ependymomas, supratentorial ependymomas, subependymomas, spinal ependymomas and myxopapillary ependymomas (which mainly occur in or along the conus medullaris and filum terminale).
The fossa posterior ependymomas are problaby the best known members of the ependymoma family. Fossa posterior ependymomas occur in children and adults and typically arise in the fourth ventricle.
Supratentorial ependymomas are less frequent, occur mainly in children and young adults, and are often located extraventricularly in the supratentorial brain parenchyma (strangely enough, the theory is that embryonic ependymal cells get trapped in the developping brain and later develop into intraparenchmal ependymomas). Supratentorial ependymomas have no typical imaging features, they can look a bit like anything making them very difficult to diagnose radiologically. I always consider supratentorial ependymoma when I’m dealing with a very strange looking supratentorial tumor in a child or adolescent and have no idea what it could be. If it’s a “I have no idea whatsoever, doesn’t look like any tumor I know” kinda tumor –> consider putting “supratentorial ependymoma” in your differential :).
Subependymomas are very benign intraventricular tumors found mainly in the frontal horn or fourth ventricle of middle aged and elderly adults. They are generally non-enhancing.

To Summarize:
This short post provided you with a quick overview of the different types of gliomas and (glio)neuronal tumors. Main point of this post is to illustrate the “the glioma” doesn’t exist .There isn’t just one glioma. The term glioma refers to a very large group of tumors that can be completely benign or highly malignant, and the kind of you gliomas you’ll encounter depends a lot on the age of the patient. As a consequence, describing a tumor as a “low grade glioma” isn’t saying much, the tumor could still be anything.
Be careful when describing a tumor as a “low-grade glioma”. Some diffuse gliomas, like astrocytoma or oligodendrolgioma, may be low grade (WHO 2), but these tumors still grow (slowly, but they grow). Surgery is not always curative due to the infiltrative growth patttern of the tumor and they have a tendency to undergo malignant transformation. The term “low grade glioma” makes a tumor seem innocent, but they aren’t always, keep that in mind.
I only provided a brief overview in this short post, but several of these tumors will be discussed in more detail in future posts. For now, I hope you got an idea of the heterogeneity of this group of tumors and got introduced to some of it’s members. A final non-exhaustive overview is found in the figure below.

A very useful and simple review
Thank you